What is Autoimmunity?
Autoimmunity is the body attacking itself.
What does that mean? In autoimmune conditions, the immune system is confused and starts trying to fight off substances and tissues that are actually “self.”
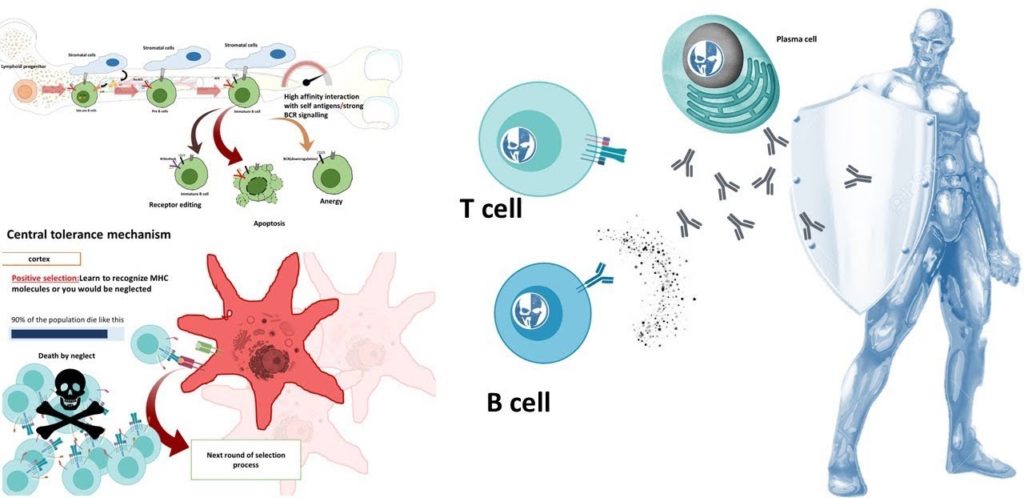
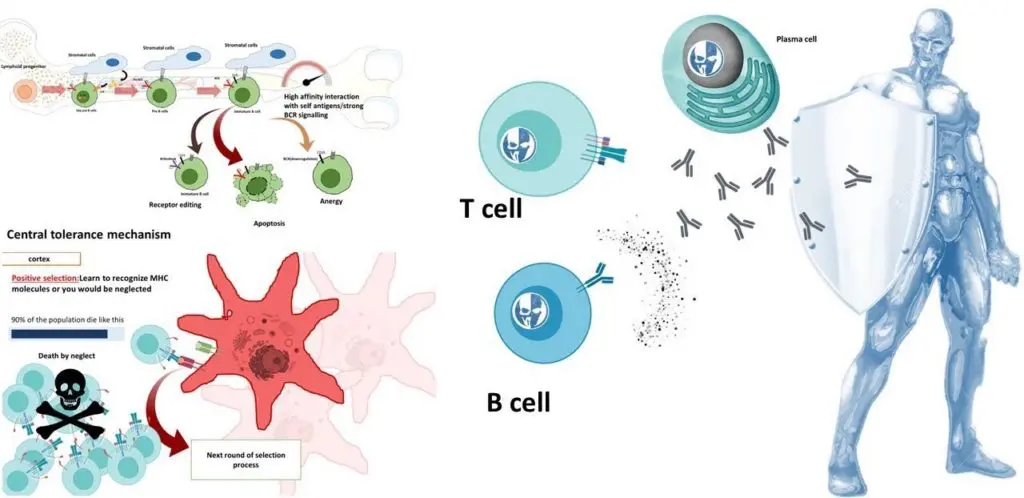
The immune system can’t tell the difference between foreign invaders and normal cells. This causes a break in tolerance for self-antigens. When this break occurs, the body begins to mount an immune response against itself which results in inflammation, tissue damage, or destruction of healthy cells. Autoimmune disease can affect any organ including joints, skin, organs inside the body such as lungs and kidneys, muscles, blood vessels – basically anywhere there is connective tissue.
The characteristic feature of autoimmune disorders is tissue damages due to inflammatory responses to antigens.
What is an antigen?
An antigen is any substance that, when it enters the body, stimulates or “primes” the immune system to react by producing antibodies to fight the substance. Antibodies are proteins. White blood cells called B lymphocytes (B cells) produce these. Any foreign substance that triggers antibody production in the body is – an antigen. These substances can be viruses, bacteria, or other microorganisms; transplanted organs or tissues; chemicals; and even foods.
Antigens are also famous as immunogens.
Antibodies are proteins. These flow in blood plasma and tissue fluids which bind with specific antigens (substances that stimulate antibody production) to neutralize, destroy, or remove them from the body.
Why do we need antigens?
Antigens are substances that our bodies recognize as being foreign and which trigger an immune response.
Antibodies are proteins found in blood plasma and tissue fluids which bind with specific antigens (substances that stimulate antibody production) to neutralize, destroy, or remove them from the body.
Autoimmunity occurs when antibodies against antigens in “self” tissues appear in the body. This causes an inflammatory response leading to suppression of the immune system and destruction of healthy cells. This results in organ damage & disease symptoms. Any substance that stimulates antibody responses are antigen
What is Autoimmunity, exactly?
Autoimmunity is where one’s own immune system attacks itself. Autoimmune disorders occur because of the body attacking itself (Type 1) or the attack being mistargeted to healthy cells & tissues (Type 2).
When this happens in the thyroid gland, the condition is -Hashimoto’s disease.
The characteristic feature of autoimmune disorders is tissue damage. This damage occurs due to inflammatory responses to antigens.
The level of severity varies from person to person depending on numerous factors, including genetics, lifestyle habits; environmental exposures.
Symptoms may develop over time-in some cases as early as a few weeks after exposure to an antigen, but in other cases may not appear for years. In some conditions, the damage occurs quickly and severely, while in others it happens over time and is less aggressive. Autoimmunity can affect any organ including joints, skin, organs inside the body such as lungs and kidneys, muscles, blood vessels – basically anywhere there is connective tissue.
Some types of autoimmune disorders include:
- Type 1 diabetes (Juvenile Diabetes)
- Rheumatoid arthritis
- Psoriasis
- Myasthenia gravis
- Dermatomyositis
- Scleroderma
- Vitiligo
- Mixed Connective Tissue Disease
- Graves’ diseases
- Rheumatoid arthritis
- Lupus Erythematosis
- Multiple sclerosis
- Graves’ disease
- Celiac disease
- Ulcerative colitis
- Crohn’s disease
- Sjogren’s syndrome
Know about the diseases we treat at Sukhayu
What causes Autoimmune conditions?
The immune system knows well to recognize and defend the body against a vast array of potential antigens. From environmental toxins and bacteria to pollen and foods.
When an antigen enters the body, B cells produce antibodies. Antigens bind to it. And it leads it to be either destruction by other cells.
When the body incorrectly identifies its own cells and tissues as antigens, it produces these antigens. And produces antibodies against them.
The specific cause of autoimmune conditions is generally unknown. But in many cases, it appears that genetics play an important role. Type 1 diabetes, for example, children who develop the disease have a 50% chance of having a relative with some form of autoimmune disease – most commonly type 1 diabetes or celiac disease (an immune reaction to gluten).
In other diseases, such as rheumatoid arthritis, there may be no family history of the disorder. But there is a genetic component. In such cases, it’s believed that certain people lack the ability to “turn off” their immune response once it has been activated.
In addition, research has shown that environmental factors – such as certain medications, viral infections, and stressors. This can trigger the onset of autoimmune disorders in people who are genetically predisposed to develop them.
Know about: Rebel of a cell
What causes an autoimmune reaction?
Autoimmune reactions occur when our immune system makes a mistake and turns against us. Our bodies contain millions of cells. But to protect ourselves from infection we need to recognize any invaders that may cause harm. Unlike other cells in the body, identification of the cells by the body’s own proteins – human leukocyte antigens (HLA). These are ‘markers’ on the surface of all cells which distinguish between your own healthy cells and foreign invaders.
The immune system has many different types of cells. But the two key players are T-cells that recognize these ‘markers’ on infected or cancerous cells, and B-cells that produce antibodies to destroy viruses. If the body starts making antibodies against its own healthy cells, this is an autoimmune reaction. The reason for this mistake is still unclear in many cases. Although some scientists believe it may be hereditary or linked to exposure to certain environmental factors.
What are the signs?
Signs vary depending on the type of autoimmune disorder but can include some of the following
- Fatigue
- Fever
- Dry mouth
- Tingling sensations in hands or feet
- Abdominal pain
- Joint pain
- Itchy, dry, or burning eyes
- Sleep disturbances
- Muscle aches and/or weakness
- Swollen glands in the neck, armpits, or groin.
How to diagnose, Autoimmunity
Diagnosis of autoimmune diseases often depends on their symptoms which can be similar to other conditions.
For example, people with celiac disease may go years without the proper diagnosis because some of its symptoms mimic Crohn’s disease – another autoimmune condition affecting the intestines.
In addition to a complete history and physical exam, patients are likely to receive one or more of the following diagnostic tests: blood tests for antibodies that attack healthy cells; imaging scans such as an x-ray, MRI, or CT scan to check for abnormalities in the body; a biopsy to confirm a suspected diagnosis.
Treating Autoimmunity
The treatment will vary depending on the type of autoimmune disease and may include medication, lifestyle changes, or both. Some common medications used to treat autoimmune diseases include steroids, immune-suppressing drugs called immunosuppressants, and other anti-inflammatory medications such as NSAIDs (nonsteroidal anti-inflammatory drugs).
In some cases, intravenous immunoglobulin therapy – which is typically used to treat immune deficiencies – has been found helpful in treating autoimmune conditions. Lifestyle changes that can help control autoimmune disorders include: healthy diet and regular exercise stress management reducing exposure to environmental toxins
What is their prognosis?
The prognosis of autoimmune disorders varies and is dependent on the specific condition. In general, they’re often manageable conditions rather than curable ones. Some people find that over time their symptoms may decrease or disappear completely with proper treatment and lifestyle changes such as those described above. Others may be able to control symptoms without medication by adopting a healthy diet and exercise program. However, in some cases symptoms can become progressively worse despite appropriate management – these patients are often treated with surgery or other more intensive measures.
Ayurveda about autoimmunity?
Science is still in early stages of understanding autoimmunity. However, Ayurvedic medicine has its own explanation for autoimmune diseases. There are three main types of disorders in Ayurveda:
Rakta Pitta Dosha
It means as soon as the body loses some blood as a result of an accident or surgery then the blood gets transformed into poison and then attacks the live blood cells
Rakta Srot Dosha
The autoimmune disease or disorder where all the patches of Rakta (Red Blood Cells) coagulate and fall apart from its own habitat i.e., red bone marrow, and start attacking other healthy red blood cells
Visham Jwar
It is one of the complicated types of condition in Ayurveda. Wherein a person keeps on suffering from different types of infections and disorders which later result in multiple organ failures. This is also known as an autoimmune disorder where one’s body starts feeling pain without any reason. This disease can be detected by checking for Vishada roga or toxicities present in human tissues due to various causes.
Ayurveda has a very wide range of management and treatment of autoimmune diseases. Such as – Tri doshas diseases and Visham Jwar using herbs, diet changes, and Panchakarma therapies.
Ayurvedic Doshas and Autoimmunity
A person’s body has three Doshas or humors called Vata, Pitta and Kapha, which are responsible for maintaining harmony in them. Any kind of stress, depression, or anxiety can produce toxins in the body leading to autoimmunity.
Vata Dosha and Autoimmunity
Vata Dosha can be very effective in treating autoimmunity. If the immune cells are high then Vata should be decreased and if the antibodies are high then Vata should be increased.
Sometimes, to balance out the vitiated doshas completely one may need to take medicines that reduce both antibodies and Vata together called immunomodulatory drugs (IMiDs).
Pitta Dosha and Autoimmunity
Pitta Dosha should be treated with anti-inflammatory and immune-modulating drugs to balance the Pitta out. Herbal therapies can also help boost immunity and treat autoimmune conditions.
Kapha Dosha and Autoimmunity
Autoimmune patients often have high levels of toxins that can lead to immunosuppression as well as infection. They may need antibiotics, antiviral agents, or antifungal medications depending on their clinical presentation
Ojas and Autoimmunity
Ojas is a crucial element in achieving and maintaining vitality. Any kind of stress, depression, or anxiety can lead to the deficiency of Ojas. This affects the immune system eventually leading to autoimmune disorders. Ayurveda suggests different herbs, diet changes, Panchakarma therapies etc for balancing Ojas. Though there is not much research done to prove the connection between Vata and Pitta dosha with autoimmune diseases. It is still considered that balancing the three doshas can be beneficial for patients suffering from autoimmunity.
Ayurvedic Autoimmune Protocol for Treatment
Based on one’s dosha types and symptoms among autoimmunity one can follow this protocol given by Vaidya Dr. Pardeep Sharma. This protocol includes herbal therapy with medicines that have immunomodulatory effects including reducing antibodies. Toxins present inside human tissues due to various causes and modulating inflammation i.e., anti-inflammatory therapy. Treatment also includes proper dietary changes recommended by an Ayurvedic doctor.
Conclusion
Science is still in the early stages of understanding autoimmunity. However, Ayurvedic medicine has its own explanation for autoimmune diseases. There are three main types of disorders in Ayurveda: Rakta Pitta Dosha, Rakta SrotDosha, and Visham Jwar. Any kind of stress, depression, or anxiety can produce toxins in the body leading to autoimmunity. Ayurveda has a very wide range of management and treatment of autoimmune diseases using herbs, diet changes, and Panchakarma therapies.
Autoimmune disorders are generally life-long conditions that tend to worsen over time if left untreated even with optimal medical therapy. Patients face an increased risk for opportunistic infections such as viral hepatitis B and C virus (HBV/HCV), human immunodeficiency virus (HIV), tuberculosis (TB), and non-tuberculous mycobacteria (NTM). They may also have significant comorbidities associated with their autoimmune conditions. For example, both rheumatoid arthritis (RA) and type 1 diabetes mellitus are associated with an increased risk of cardiovascular disease.